Task Group 116
Radiological Protection Aspects of Imaging in Radiotherapy
Under Committee 3
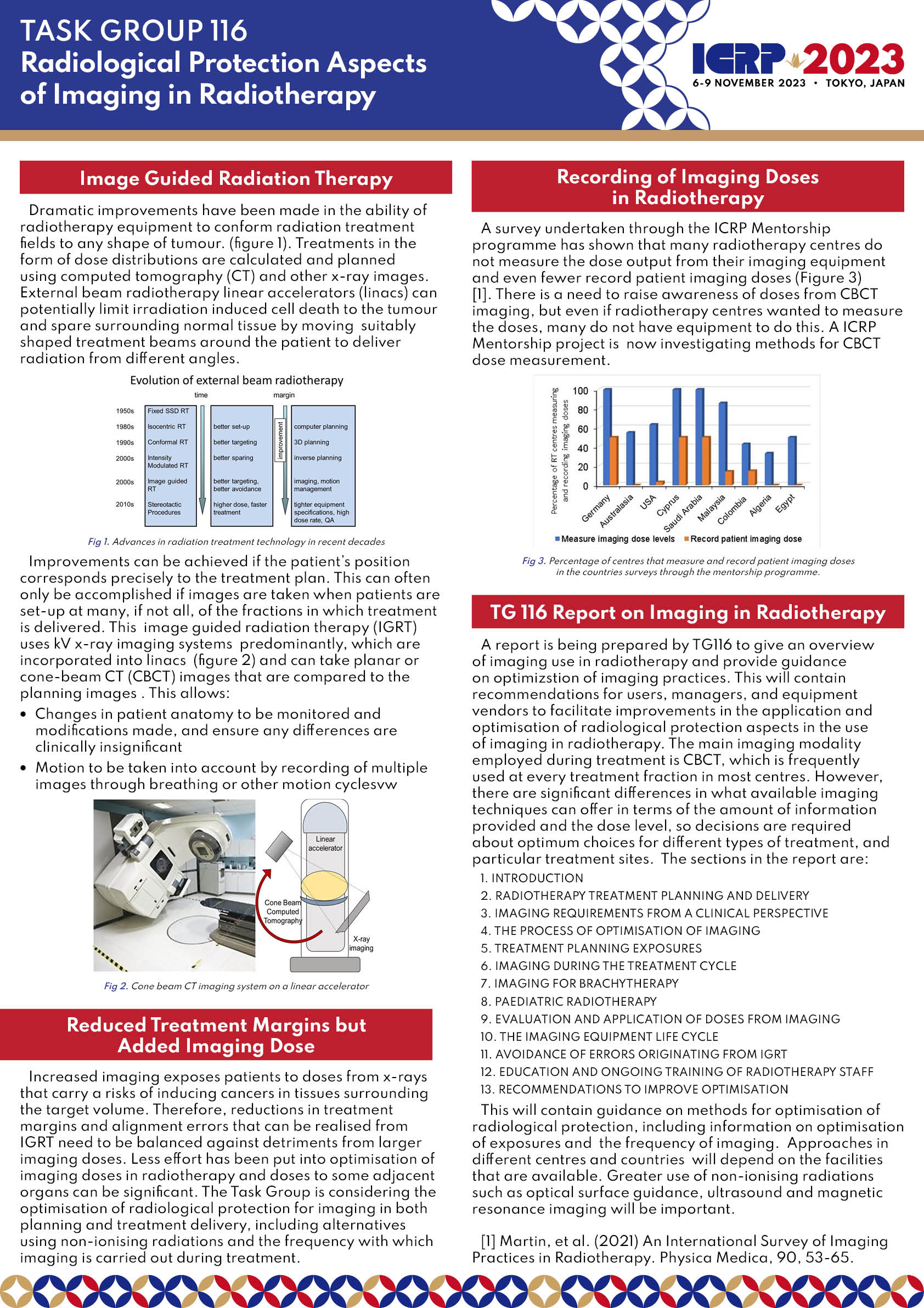
Modern radiotherapy equipment delivers radiation beams from multiple directions conformed to the shape of the target tumour to achieve a planned radiation distribution. Imaging is crucial for successful planning and delivery of this dynamic image guided radiation therapy, to provide additional accuracy in localisation of tumour volumes at the time of treatment. Imaging may be associated with each of the therapy fractions in order to adjust for tumour volumes and any movement in other organs. This is accomplished using either kV or MV orthogonal x-rays or cone beam computed tomography imaging systems integrated into linear accelerators, and enables radiation field margins surrounding the tumour to be reduced. However, if imaging is used frequently with little optimisation, doses to organs and tissues outside the planning target volume can reach tens of mGy per radiotherapy fraction and the imaging dose delivered to the tumour over the course of treatment is no longer insignificant. The use of radiography and fluoroscopy in planning brachytherapy treatment will also be considered. At the present time, practices vary between centres in imaging modalities used, the frequency of imaging, and the level of optimisation undertaken, so more guidance is needed.
This task group will provide guidance on radiological protection aspects in the use of imaging (e.g., cone beam CT, fluoroscopy) in radiotherapy. Advice will relate to optimisation of protocols for exposures carried out during the planning stages, and the frequency and level of optimisation for imaging performed for treatment guidance. The report will consider the trade-off between therapeutic advantages and additional radiation doses from imaging. The report will also examine the need for assessment of organ and tissue doses relating to imaging for communication to radiation oncologists and inclusion in the planning process.
The first draft version of the report will be made available for public consultation and discussion by the end of 2024.
ICRP 2023 Poster
| Colin Martin (Chair), University of Glasgow, United Kingdom | ||
| William Small (Vice-Chair), USA | ||
| Sebastien Gros (Member), Loyola University Medical Center, USA | ||
| Aurelie Isambert (Member), ASNR, France | ||
| Stine Korreman (Member), Denmark | ||
| Tomas Kron (Member), Peter MacCallum Cancer Centre, Australia | ||
| Choonsik Lee (Member), National Cancer Institute, USA | ||
| Thomas Merchant (Member), USA | ||
| Ngie Min Ung (Member), University of Malaya, Malaysia | ||
| Jenia Vassileva (Member), Bulgaria | ||
| Tim Wood (Member), Hull University Teaching Hospitals, United Kingdom | ||
| Abdullah Abuhaimed (Member-Mentee), King Abdulaziz City for Science and Technology, Saudi Arabia | ||
| Buthaina Al Ameri (Member-Mentee), Federal Authority for Nuclear Regulation, United Arab Emirates | ||
| Zakiya Al Rahbi (Member-Mentee), Oman | ||
| Anson Cheung Ho Yin (Member-Mentee), China | ||
| Ana Cravo Sá (Member-Mentee), Portugal | ||
| Mario Djukelic (Member-Mentee), GenesisCare, Australia | ||
| Mirta Dumancic (Member-Mentee), Gerald Bronfman Department of Oncology, McGill University, Montréal QC, Canada | ||
| Hein Fourie (Member-Mentee), South Africa | ||
| Marianna Koutrouli (Member-Mentee), Newcastle upon Tyne Hospitals NHS Foundation Trust, United Kingdom | ||
| Anja Lazovic (Member-Mentee), Serbia | ||
| Runcheng Liang (Member-Mentee), China Institute for Radiation Protection, China | ||
| Aliaksandr Miadzvetski (Member-Mentee), N.N. Alexandrov National Cancer Centre of Belarus, Belarus | ||
| Francisco Mosquera-Pena S�nchez (Member-Mentee), Spain | ||
| Lavanya Murugan (Member-Mentee), Rajiv Gandhi Government General Hospital and Madras Medical College, Chennai, India | ||
| Piotr Pankowski (Member-Mentee), Department of Nuclear Physics and Radiation Safety, Faculty of Physics and Applied Informatics University of Lodz, Poland | ||
| Maria Cristina Plazas (Member-Mentee), Universidad Nacional de Colombia, Colombia | ||
| Hossam Ragab (Member-Mentee), Senior Medical Physicist at Warith International Cancer Institute, Iraq | ||
| Yiannis Roussakis (Member-Mentee), German Oncology Center, Cyprus | ||
| Snezana Vostinic (Member-Mentee), Serbia | ||
| Daniel Berger (Representative), International Atomic Energy Agency, AUSTRIA |